Case study: Measuring wellbeing program effectiveness
What 3 years of data reveals about a large regional health plan’s employee compliance wellbeing program
WellSpark would be hard-pressed to find a client with a better understanding of the importance of supporting employee health and wellness than a large regional health plan. WellSpark has engaged the health plan’s eligible workforce in a custom wellness program focused on early intervention to address emerging health risks and support chronic condition self-management.
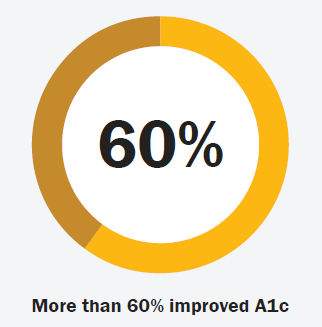
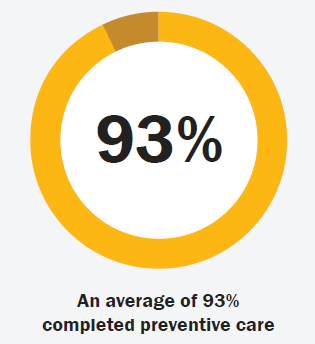
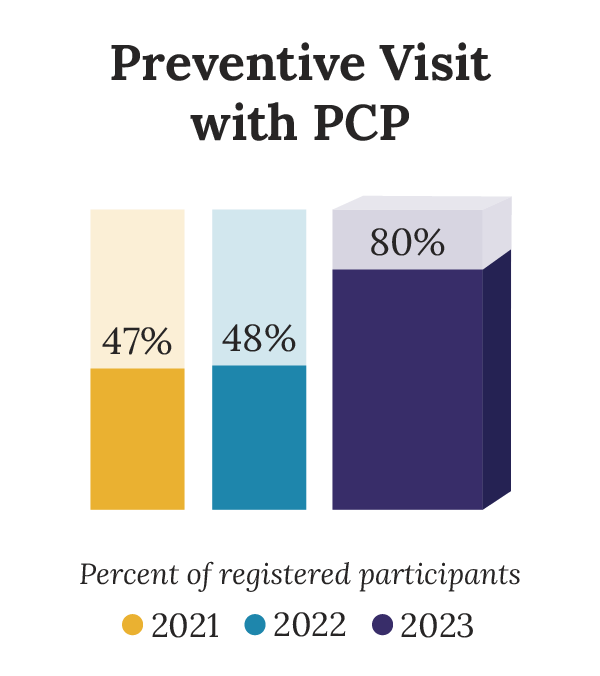
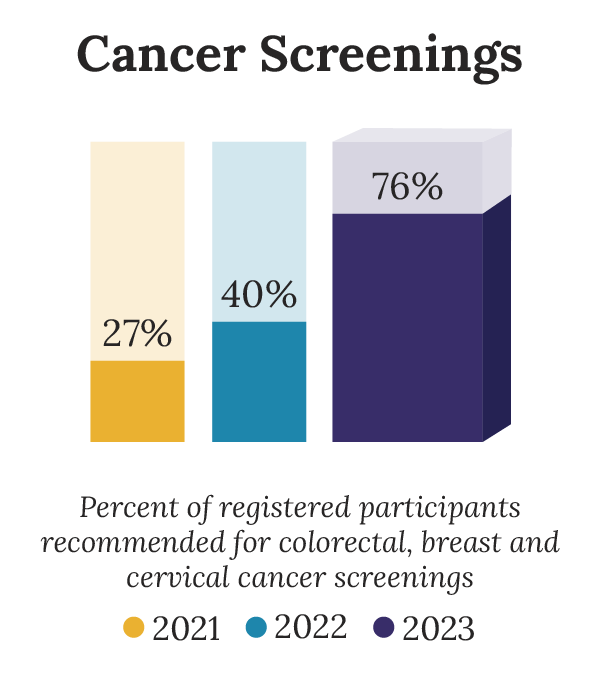
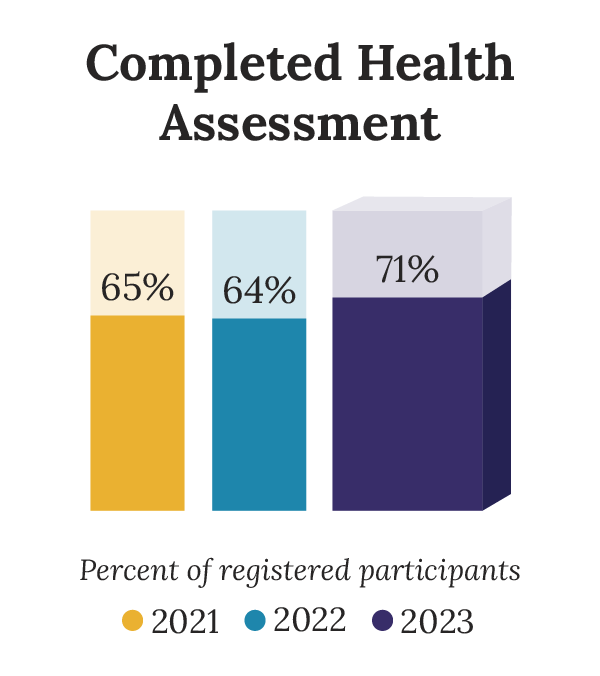
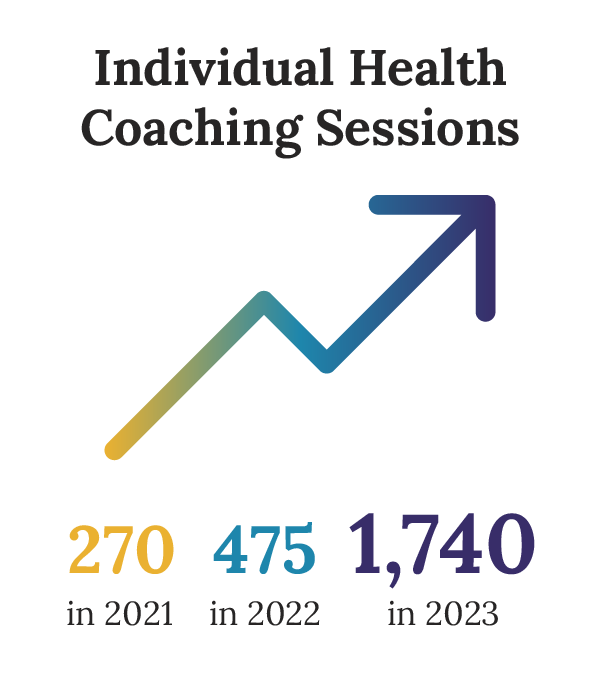
Building an organizational culture that supports employee health and wellbeing takes consistent effort to educate and engage eligible participants in the wellness benefits available. Employee participation is an important key to success for any employee wellness program; and medical checkups and wellness screenings are an important part of preventive care. Over the past three years, the data validates the significant increase WellSpark has achieved in the participation, completion of recommended screenings and engagement in health coaching programs for this health plan client.
About the client and the program:
- This program is administered across several business units of a large regional health plan provider for its more than 2000 eligible employees.
- The compliance program includes 24/7 access to a digital wellness platform, individual and group health coaching, group challenges, webinars, and diabetes and chronic condition prevention programs.
- Prior to 2023 for the majority of its business units, the health plan offered money-back incentives to employees for participating in the wellbeing program and completing certain activities.
- Beginning in 2023, the health plan offered preferred health insurance premiums to the eligible population in all of its business units. Additionally, with the help of WellSpark, the health plan increased the communications promoting the program and added one-to-one outreach to those at risk of chronic conditions.
- Registration in the wellness program has increased yearly by an average of 22%.

What picture does this data paint?
It’s not an exaggeration to say that employers who provide employees with health and wellness programs that support the employee’s desire for behavior change save lives. This aggregate data across three years shows this health plan provider has increased the number of its employees who have completed preventive care screening. At the end of 2023, an average of 80% of the program participants completed a preventive care visit with a primary care physician (PCP).
The Centers for Disease Control and Prevention estimates preventive care services could save more than 100,000 lives in the U.S. each year.1 A new study announced in July led by researchers at the American Cancer Society found that 40% of cancer cases and about one-half of all cancer deaths in adults 30 years old and older in the United States are attributable to modifiable risk factors.2
An article in the February 2024 Mayo Clinic journal PROCEEDINGS: Innovations, Quality & Outcomes highlighted the burden of chronic disease on society. The cost of chronic disease worldwide is estimated to reach $47 trillion by 2030. Many preventable chronic diseases can be modified by addressing four major risk factors: physical inactivity, poor nutrition, tobacco use, and excessive alcohol. Lifestyle behavior change and nonmedical factors that influence health (social determinants of health) are critical to addressing rising rates of chronic disease.3
The National Association of Chronic Disease Directors estimates that 60% of American adults have at least one chronic condition, and the average annual spend for one employee with at least one chronic condition is $6,032.4
Providing support to those employees who are ready for the type of lifestyle change that can positively impact their health and wellbeing benefits not only those employees but also the communities where those individuals work, live and play.
About WellSpark
WellSpark Health is a national wellbeing provider headquartered in Farmington, Connecticut that couples health coaching with the virtual modalities desired by today’s workforce. Since 2013, WellSpark has partnered with a broad range of public and private sector employers, providing engaging coaching and disease prevention programs through a life-dimensional approach that supports the whole employee while creating a supportive workplace culture. Employee participation from those who need it most is what matters. That’s where WellSpark’s consultative and customizable approach truly delivers.
Sources:
[1] Center for Disease Control and Prevention (2020) Access to Health Care. Retrieved August 6, 2024, from https://archive.cdc.gov/#/details?q=cdc.gov/vitalsigns/healthcareaccess/&start=0&rows=10&url=https://www.cdc.gov/vitalsigns/healthcareaccess/index.html
[2] American Cancer Society (2024). Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. Retrieved August 6, 2024, from https://pressroom.cancer.org/releases?item=1341#
[3] Mayo Clinic Journal PROCEEDINGS. The Burden of Chronic Disease. Retrieved August 6, 2024, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10830426/#
[4] National Association of Chronic Disease Directors (2022). Commentary on Chronic Disease Prevention in 2022. Retrieved August 6, 2024, from chronicdisease.org/commentary-chronic-disease-prevention-2022-david-hoffman/
Any examples are not intended to guarantee that an organization or individual will achieve the same or similar results. Each organization’s or individual’s success depends on many factors.